They faced the coronavirus in the hardest moments, when the virus was still a real unknown. They did it without protection, in fear of not knowing if they were going to infect themselves or their loved ones. For a few months they received the applause from the window of many Spaniards, which helped them cope with the overload they faced on a day-to-day basis. Today, two years later, they continue to suffer from stress and anxiety, and mental problems have appeared among health workers more than any other population group, while their working conditions remain as restrictive only in early 2020.
health professionals suffered from a disorder related to anxiety (22,5%), panic attacks (24%), post-traumatic stress disorder (22,2%), depression (28,1%) or drug addiction (6,2%) ), compared to 23,6% of the general population. These are the data that emerge from the Mindcovid study, financed by the Carlos III Health Institute and coordinated by the Hospital del Mar Biomedical Research Institute (IMIM) and which analyzes the influence that the pandemic has had in the last two years, in addition to the population, in 10.000 health professionals.
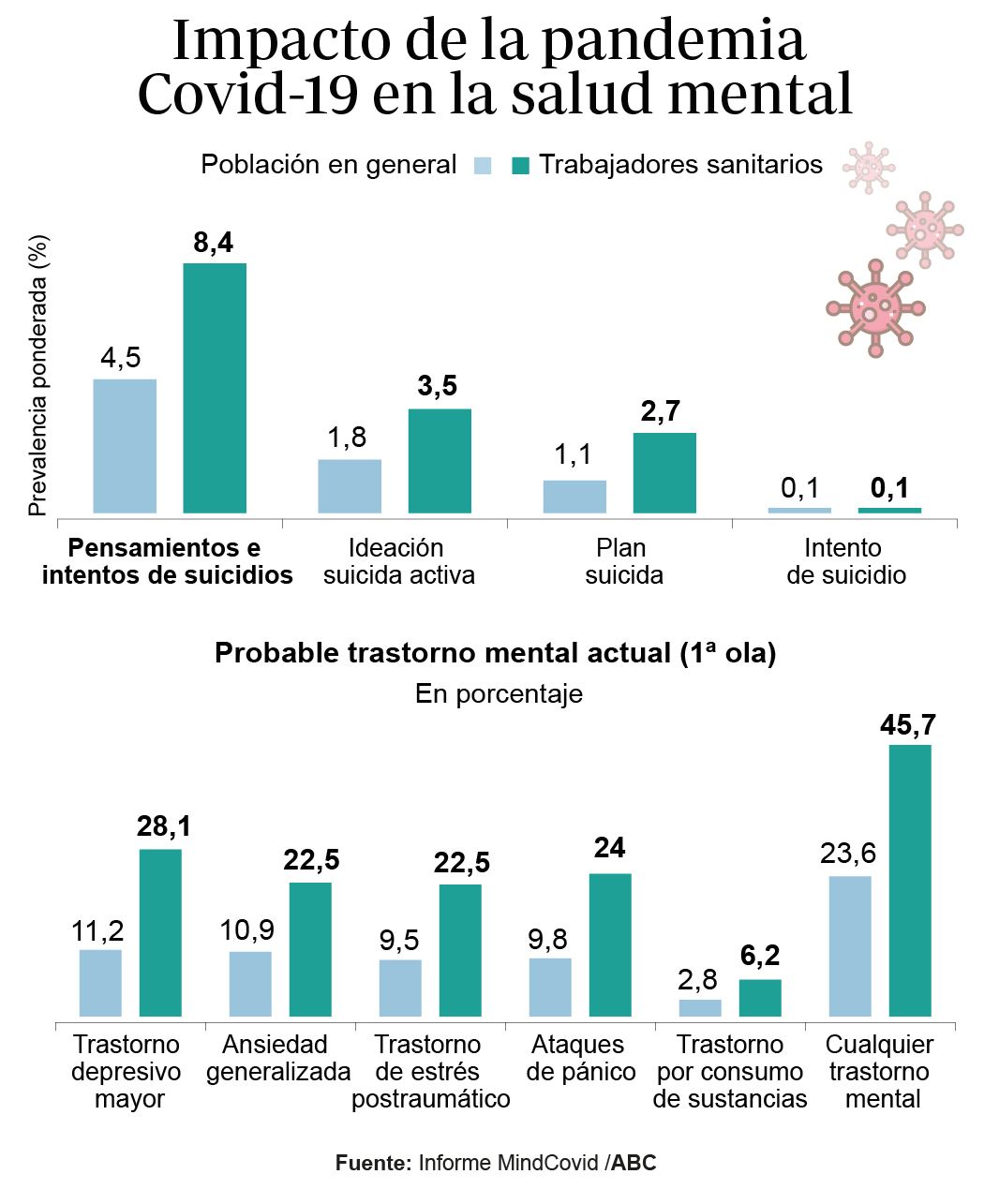
One of the most relevant data that emerges from the analysis is that of the 45,7% of these health workers who suffered from some disorder, a quarter (around 14,5%) also suffered from a significant disability that limited their work. "Among those who care for patients, there is a very high probability that they suffer from a mental disorder, and a significant proportion is disabling," explained Jordi Alonso, principal investigator of the study, during the presentation of the study on Friday. .
twice the incidence
A direct consequence of the mental health status of these professionals is that the research found that up to 8,4% of health workers presented suicidal ideation or behavior in the 30 days prior to the survey, while in the rest of the general population, this rate was 4,5. % Among those who even had a plan designed to commit suicide, the rate is 2,7% (1,1% outside the health field). Factors that precipitate these problems include being young, female, pre-existing mental illness, and poor working conditions, such as lack of communication, supervision, and protection, as well as loss of income.
It was last summer when, after a series of suicides of Internal Medicine residents (MIR), society turned its attention to this forgotten subject that is still taboo. It was then, after learning more details about what happened, that David -fictitious name- was recognized in what had happened to him a few years before, being also a resident. «J'ai I remarked that j'avais de la difficulté à faire mon travail, à me concentrate et à faire attention, alors j'ai été grondé ou réprimandé, j'ai augmenté le stress et j'ai tout empiré», dit- Him. But these difficulties were not limited to work, but also to personal: «The irritability was installed and in the little free time I had I was so tired that I did not want to go out, I just wanted to be at home». to rest.
David broke up with his partner at that time and acknowledges the "weak" support among non-care staff, due to the stigma of mental health. His problem was resolved with the intervention of the Comprehensive Support Program for the Sick Physician of the College of Physicians, although since then he has not been able to stop the medication or follow-up. He abandoned his specialty -Family and Community Medicine- and developed his professional career in the field of occupational health.
Yes, he was in the eye of Hurricane Erika -fictitious name-, in the midst of a pandemic in a Madrid hospital. There she was in intensive care in intensive care until the day she couldn't take it anymore. “I called my mom and told her that she couldn't take it, that she didn't want to go back another day. The days she was free she didn't even want to set foot in the city of Madrid, she just wanted to go far away”. When she was discharged for depression, she wondered why she couldn't take it anymore "if 50-year-olds put up with it," and she chastised herself "for being so sweet." So he was medicated for months, taking anxiolytics and antidepressants, and today, almost a year after leaving the front lines and even starting economics studies, he still needs sleeping pills. . “It is that you cannot stand this pressure, nor the treatment, because you feel that you are not recognized, neither by society, nor economically. You give a lot and you get nothing in return,” he says.
take care of others
From the AMYTS doctors' union, Ángel Luis Rodríguez, head of the mental service, explains that at the first moment of the pandemic, the health workers blamed anxiety above all else. "They were afraid of bringing the virus home, and this caused problems with insomnia and irritability, as well as making it difficult for them to relate to the rest of their classmates," he reveals. “After that moment of a lot of adrenaline in the blood, they went into depression, with a lack of enthusiasm, and cases of 'burnout' or 'burnout' appeared, the most characteristic symptom currently with post-stress.
But among those who have used these services, it seems that 3,5% have thought of suicide as a way out of a situation that they believe they can no longer control, even with concrete ideas of how and when they would do it. As he explains, "among doctors there is a stigma of having mental health problems" because it seems that "they cannot do their job well" of caring for others.

The MIR, the weakest link
Fed up, lazy and tired, this is how Alex Mayer, vice president of the AME, defines the limit situation that these professionals live. In his case, he represents the resident doctors, "the youngest, with less professional experience", and therefore, "the most negligent". According to him, it is not just about asking for psychological help, but also "improving conditions, improving wages and stabilizing contacts."
Along the same lines, Alejandro Cuéllar, coordinator of FSE Unida, tells how the pressure reaches such a point that these professionals resort to self-medication. “On the one hand, the administration is not helping us, and on the other, the social stigma of feeling weak still prevails” when acknowledging that this limiting mental health problem exists.
